Hidden Encephalitis: What It Is and Why It’s More Common Than You Know
Hidden encephalitis is a form of encephalitis that’s often missed and therefore undiagnosed; yet, it causes a variety of symptoms and health concerns. Fortunately, eating an anti-inflammatory diet, focusing on nutritional therapy, practicing stress relieving techniques, and more offer effective natural treatment options.

Hidden encephalitis is a form of encephalitis that’s often missed and therefore undiagnosed; yet, it causes a variety of symptoms and health concerns. Fortunately, eating an anti-inflammatory diet, focusing on nutritional therapy, practicing stress relieving techniques, and more offer effective natural treatment options.
Encephalitis is a term that some people have heard of, research shows that 78 percent of the world’s population doesn’t know what it is. And of the estimated 22 percent who have heard of it, only a very small amount actually understand what all it entails. And that’s because it can manifest as a variety of symptoms and health complications.
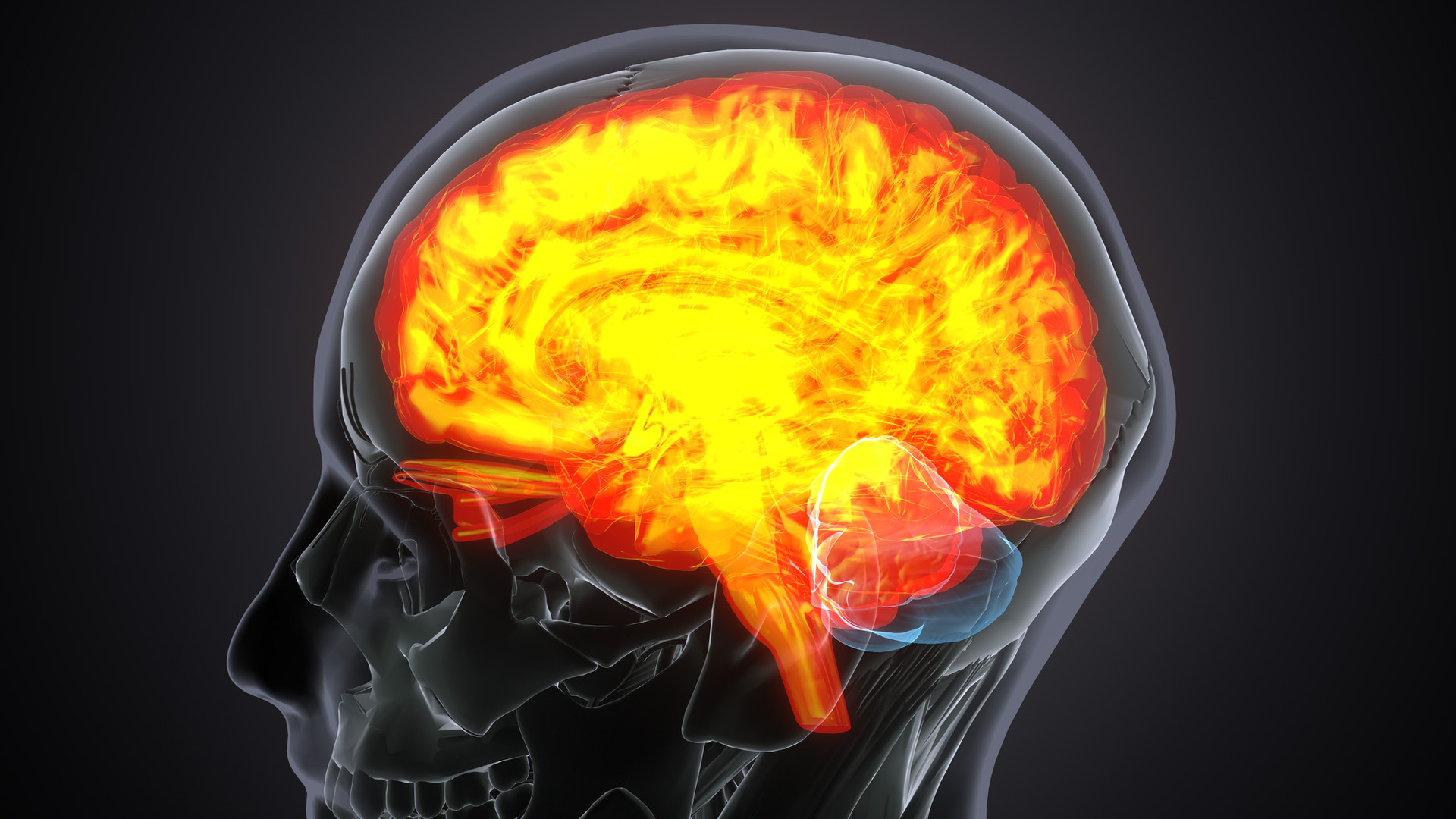
At its core, encephalitis is a condition characterized by inflammation of the brain, and many have been taught that it’s quite rare. And if we’re talking about “true encephalitis,” which is a brain infection (such as meningitis-related encephalitis), that’s correct. It’s estimated that out of 100,000 people, only 10 to 15 are diagnosed each year.
But the truth is actually quite shocking: The reality is that there is a lesser-known form of encephalitis known as hidden encephalitis that often goes undiagnosed. And it’s much more common than you might think. In fact, it’s very likely you or someone you love has been affected at some point—even if you didn’t realize it. And every day that the diagnosis is missed is one step further away from living a life full of health and vitality.
So, let’s take a closer look at hidden encephalitis and explore what it is, the top symptoms, causes, and the common health conditions it’s associated with. Then we’ll discuss the importance of diagnosing hidden encephalitis and review some of the best natural treatment options known to fight brain inflammation and support full-body health.
What Is Encephalitis?
In order to better understand hidden encephalitis, first we must quickly discuss encephalitis.
Encephalitis is a very serious (and sometimes deadly) medical condition that can have a variety of causes, including bacterial or viral infections, autoimmune disorders, exposure to toxins, injuries, and certain lifestyle factors. It often presents as a headache and/or stiff neck and may result in mental confusion and even seizures.
Viral infections, such as herpes simplex virus, West Nile virus, and enteroviruses, are common culprits behind encephalitis. These viruses can enter your central nervous system and trigger an immune response that results in the characteristic swelling and irritation of your brain tissue.
But encephalitis can also be caused by autoimmune disorders, which can cause your body’s immune system to mistakenly attack your healthy brain cells, leading to inflammation.
In addition to infectious and autoimmune causes, environmental factors can also play a role in the development of encephalitis. Exposure to certain toxins, such as lead or pesticides, can trigger an inflammatory response in your brain. And specific lifestyle factors, including having a weakened immune system due to chronic stress or poor nutrition, can make you more susceptible to developing encephalitis.
Finally, head injuries, even seemingly minor ones, can trigger hidden encephalitis. How? The impact from a head injury can disrupt your blood-brain barrier, allowing inflammatory molecules to enter your brain and initiate a cascade of inflammatory responses.
It’s crucial to be aware of the different factors that can contribute to encephalitis so that you can take preventive measures and quickly seek medical intervention, if needed.
What Is Hidden Encephalitis?
Hidden encephalitis is different from “true encephalitis” because it’s a condition that often presents with nonspecific symptoms such as fatigue, headaches, and mild cognitive impairment. And these are symptoms that can easily be mistaken for other common ailments, which often leads to a delay in diagnosis and treatment.
In some cases, people with hidden encephalitis may experience subtle changes in mood or behavior, which can further complicate the ability to receive the correct diagnosis.
Now, it’s important to note that just as with true encephalitis, hidden encephalitis can be triggered by many different factors, including viral infections, autoimmune disorders, environmental toxins, injuries, and lifestyle factors, such as poor gut health.
Similarly, the brain inflammation associated with this condition can disrupt your normal neurological function, potentially leading to long-term complications if it’s missed and left untreated, which it often is. And that’s why hidden encephalitis is so dangerous and why it’s referred to as “hidden.”
Early detection and intervention are crucial in managing hidden encephalitis and preventing further damage to your brain.
Symptoms of Hidden Encephalitis
So, how do you know if you have hidden encephalitis?
While the symptoms may be subtle at first, such as experiencing mild cognitive difficulties or unexplained fatigue, the long-term consequences of untreated hidden encephalitis can be significant.
Research shows that chronic low-level inflammation in the brain can lead to a range of neurological and psychiatric disorders, including depression, anxiety, and even cognitive decline.
In addition to its impact on your mental health, hidden encephalitis can also affect your physical well-being. Studies have shown that ongoing inflammation in your brain may contribute to systemic inflammation throughout your body, potentially increasing your risk of developing other inflammatory conditions such as autoimmune diseases and even heart disease.
It’s easy to see why it’s so important to identify and treat hidden inflammation. While symptoms may vary from person to person, here are some of the most common symptoms of hidden encephalitis:
- Difficulty with concentration
- Trouble paying attention
- Struggling to process information
- Confusion or disorientation that disrupts daily activities
- Mood changes
- Sleep disturbances
- Headaches
- Seizures and other neurological abnormalities (in more severe cases)
Remember that hidden encephalitis can often be challenging to diagnose because the symptoms may be subtle and even mimic other conditions. For example, some cognitive difficulties such as memory problems and difficulty concentrating can easily be attributed to stress or lack of sleep. Likewise, mood changes and sleep disturbances may be mistaken for common mental health issues such as anxiety or depression.
As a result, it’s imperative to seek prompt medical attention and undergo the appropriate testing if you’re experiencing the symptoms listed above.
Hidden Encephalitis & Common Health Conditions
Because it can be tough to connect the symptoms above with hidden encephalitis, it’s important to know hidden encephalitis. These include post-COVID syndrome, fibromyalgia, chronic fatigue syndrome, chronic pain, and chronic traumatic encephalopathy.
Let’s take a closer look at each of these common health conditions and their links to hidden encephalitis.
Post-COVID Syndrome
Post-COVID syndrome, also known as long COVID, refers to a condition where people experience persistent COVID symptoms even after recovering from the virus. In fact, it’s reasonable to believe that hidden encephalitis may be one of the underlying causes of the lingering symptoms in post-COVID syndrome.
Hidden encephalitis can manifest in different ways in people with post-COVID syndrome. That’s because inflammation in the brain, a hallmark of encephalitis, can lead to different cognitive impairments such as memory loss, difficulty concentrating, and brain fog.
Additionally, people with hidden encephalitis may experience mood disturbances, such as depression and anxiety, further impacting their quality of life.
Fibromyalgia
Fibromyalgia is a chronic syndrome characterized by widespread pain, fatigue, and tenderness in certain areas of your body. But you may be surprised to learn that research suggests a strong link between hidden encephalitis and fibromyalgia.
Specifically, several studies have shown that people with fibromyalgia show signs of brain inflammation, particularly involving the activation of glial cells.
One study used imaging tests (MRI/PET scans) to analyze brain activity and revealed that those with fibromyalgia had higher levels of a protein associated with glial cells, indicating brain inflammation. The study found that the higher levels of the protein were most pronounced in people experiencing severe fatigue, suggesting a direct connection between brain inflammation and fibromyalgia symptoms
Ready to feel like you again?
* Your next step toward feeling better starts today. At The Dearing Clinic we make it simple to get started with care that truly fits your life. Book your visit now and let’s design a plan that restores your energy, relieves your pain, and helps you enjoy more of what matters most.